中国防痨杂志 ›› 2024, Vol. 46 ›› Issue (10): 1273-1282.doi: 10.19982/j.issn.1000-6621.20240207
闫红璇1, 袁金锋2, 王艺霖2, 逄宇2( ), 高孟秋1(
), 高孟秋1( )
)
收稿日期:2024-05-25
出版日期:2024-10-10
发布日期:2024-09-29
通信作者:
高孟秋,Email:基金资助:
Yan Hongxuan1, Yuan Jinfeng2, Wang Yilin2, Pang Yu2( ), Gao Mengqiu1(
), Gao Mengqiu1( )
)
Received:2024-05-25
Online:2024-10-10
Published:2024-09-29
Contact:
Gao Mengqiu,Email:Supported by:摘要:
宿主导向治疗(host-directed therapy, HDT)是一种新的结核病辅助治疗方法,它针对宿主细胞而非病原体,利用调节宿主免疫应答反应来对抗感染。当药物与抗结核药物联合应用时,有助于增强化学药物疗效、缩短治疗时间、改善免疫病理损伤和减少耐药性产生等。笔者综述了结核病HDT候选药物的常见作用机制,并列举了目前正在研究的HDT候选药物,为寻找新型有效的抗结核治疗药物提供参考依据。
中图分类号:
闫红璇, 袁金锋, 王艺霖, 逄宇, 高孟秋. 结核病宿主导向治疗的研究进展[J]. 中国防痨杂志, 2024, 46(10): 1273-1282. doi: 10.19982/j.issn.1000-6621.20240207
Yan Hongxuan, Yuan Jinfeng, Wang Yilin, Pang Yu, Gao Mengqiu. Advances in the host-directed therapy of tuberculosis[J]. Chinese Journal of Antituberculosis, 2024, 46(10): 1273-1282. doi: 10.19982/j.issn.1000-6621.20240207
表1
目前正在研究的结核病HDT候选药物
| 名称 | 机制 | 研究阶段 | 人/动物 | 参考文献 |
|---|---|---|---|---|
| 帕唑帕尼 | 抑制VEGF,影响肉芽肿 | 临床前 | 斑马鱼 | [ |
| 多西环素 | 抑制MMPs,影响肉芽肿 | 临床试验Ⅲ期 | 结核病患者 | [ |
| 伊马替尼 | 阻断PI3K/Akt/mTOR,促自噬 | 临床前 | 小鼠 | [ |
| 雷帕霉素 | 抑制mTOR,促自噬 | 临床前 | 小鼠 | [ |
| 依维莫司 | 抑制mTOR,促自噬 | 临床试验Ⅱ期 | 结核病患者 | [ |
| 硝唑尼特 | 抑制NQO1,促自噬 | 临床前 | 细胞 | [ |
| 卡马西平 | 激活AMPK,促自噬 | 临床前 | 小鼠 | [ |
| 氟西汀 | 促进JNK途径,促自噬 | 临床前 | 小鼠 | [ |
| 吉非替尼 | 抑制p38MAPK,促自噬 | 临床前 | 小鼠 | [ |
| 他莫昔芬 | 促溶酶体输送,促自噬 | 临床前 | 斑马鱼 | [ |
| 巴多昔芬 | 增强ROS产生,促自噬 | 临床前 | 细胞 | [ |
| 维生素D3 | 上调自噬相关基因,促自噬 | 临床试验Ⅲ期 | 结核病患者 | [ |
| 维拉帕米 | 抑制钙离子外排泵Rv1258,促自噬 | 临床前 | 细胞 | [ |
| 洛哌丁胺 | 诱导ATG16L1基因的表达,促自噬 | 临床前 | 小鼠 | [ |
| 维生素B1 | 抑制PPAR-γ,增强巨噬细胞杀伤力 | 临床前 | 细胞 | [ |
| 霉菌素 | 抑制PPAR-γ,增强巨噬细胞杀伤力 | 临床前 | 小鼠 | [ |
| 二甲双胍 | 诱导CD8+T细胞免疫代谢回路;抑制mTOR,促自噬;调节炎症反应 | 临床试验Ⅱ期 | 结核病患者 | [ |
| 比阿培南 | 增强T淋巴细胞对炎症亚群的极化 | 临床前 | 小鼠 | [ |
| 氯法齐明 | 阻断Kv1.3钾通道促进中央记忆型T细胞产生 | 临床前 | 小鼠 | [ |
| 沙奎那韦 | 增加T淋巴细胞的启动和增殖 | 临床前 | 细胞 | [ |
| 布洛芬 | 抑制COX,抑制过度炎症 | 临床试验Ⅱ期 | 结核病患者 | [ |
| 阿司匹林 | 抑制COX,抑制过度炎症 | 临床试验Ⅱ期 | 结核病患者 | [ |
| 塞来昔布 | 抑制COX,抑制过度炎症 | 临床前 | 小鼠 | [ |
| 依托考昔 | 抑制COX,抑制过度炎症 | 临床试验Ⅰ期 | 结核病患者 | [ |
| 美洛昔康 | 抑制COX,抑制过度炎症 | 临床试验Ⅲ期 | 结核病患者 | [ |
| 西洛他唑 | 抑制PDEs,减少巨噬细胞活化和TNF-α表达,抑制过度炎症 | 临床前 | 小鼠 | [ |
| 西地那非 | 抑制PDEs,减少巨噬细胞活化和TNF-α表达,抑制过度炎症 | 临床前 | 小鼠 | [ |
| 罗氟司特 | 抑制PDEs,减少巨噬细胞活化和TNF-α表达,抑制过度炎症 | 临床前 | 小鼠 | [ |
| 齐留通 | 抑制5-LOX,抑制过度炎症 | 临床前 | 小鼠 | [ |
| 阿托伐他汀 | 抑制胆固醇、Rho蛋白合成,抑制过度炎症;诱导自噬 | 临床试验Ⅱ期 | 结核病患者 | [ |
| 瑞舒伐他汀 | 抑制胆固醇、Rho蛋白合成,抑制过度炎症;诱导自噬 | 临床试验Ⅱ期 | 结核病患者 | [ |
| N-乙酰-L-半 胱氨酸乙酯 | 抑制宿主氧化反应,调节炎症 | 临床试验Ⅱ期 | 结核病患者 | [ |
| 舍曲林 | 抑制Ⅰ型干扰素反应,减轻过度炎症 | 临床前 | 小鼠 | [ |
| 依那西普 | 抑制TNF-α,减轻过度炎症 | 临床前 | 小鼠 | [ |
| 托法替尼 | 抑制JAK,调节炎症 | 临床前 | 小鼠 | [ |
| 帕考珠单抗 | 抗IL-4单克隆抗体,调节炎症 | 临床试验Ⅱ期 | 结核病患者 | [ |
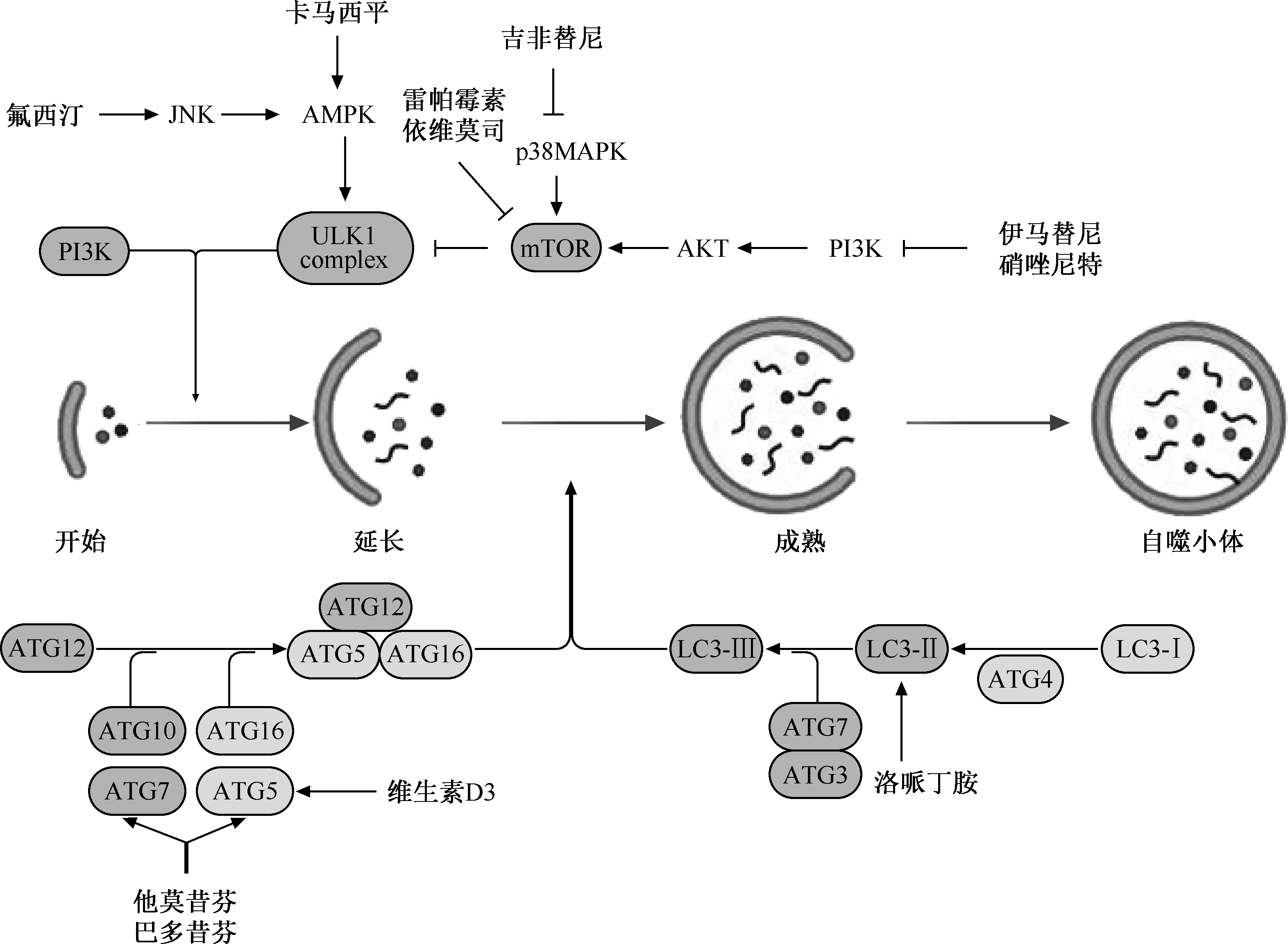
图2
增强宿主天然免疫的结核病HDT候选药物作用机制 注 JNK:c-Jun氨基末端激酶;AMPK: 腺苷酸激活蛋白激酶;p38MAPK:p38丝裂原活化蛋白激酶;PI3K:磷脂酰肌醇3激酶;ULK1 complex:UNC-51样激酶1复合物;mTOR:雷帕霉素靶蛋白;AKT:蛋白激酶B;ATG12:自噬相关基因12;ATG10:自噬相关基因10;ATG7:自噬相关基因7;ATG5:自噬相关基因5;ATG16:自噬相关基因16;ATG3:自噬相关基因3;ATG4:自噬相关基因4;LC3-Ⅰ:自噬微管相关蛋白轻链3-Ⅰ;LC3-Ⅱ: 自噬微管相关蛋白轻链3-Ⅱ;LC3-Ⅲ:自噬微管相关蛋白轻链3-Ⅲ
| [1] | Wallis RS, O’garra A, Sher A, et al. Host-directed immunotherapy of viral and bacterial infections: past, present and future. Nat Rev Immunol, 2023, 23(2):121-133. doi:10.1038/s41577-022-00734-z. |
| [2] | Huang X, Lowrie DB, Fan XY, et al. Natural products in anti-tuberculosis host-directed therapy. Biomed Pharmacother, 2024, 171:116087. doi:10.1016/j.biopha.2023.116087. |
| [3] | 王丽, 杨恩卓, 沙巍, 等. 结核病免疫治疗的研究进展. 中国防痨杂志, 2022, 44 (10): 1079-1084. doi:10.19982/j.issn.1000-6621.20220194. |
| [4] |
Hawn TR, Shah JA, Kalman D. New tricks for old dogs: countering antibiotic resistance in tuberculosis with host-directed therapeutics. Immunol Rev, 2015, 264(1):344-362. doi:10.1111/imr.12255.
pmid: 25703571 |
| [5] | Wallis RS, Maeurer M, Mwaba P, et al. Tuberculosis-advances in development of new drugs, treatment regimens, host-directed therapies, and biomarkers. Lancet Infect Dis, 2016, 16(4): e34-e46. doi:10.1016/S1473-3099(16)00070-0. |
| [6] | Cubillos-Angulo JM, Nogueira BMF, Arriaga MB, et al. Host-directed therapies in pulmonary tuberculosis: Updates on anti-inflammatory drugs. Front Med (Lausanne), 2022, 9:970408. doi:10.3389/fmed.2022.970408. |
| [7] | Oehlers SH, Cronan MR, Scott NR, et al. Interception of host angiogenic signalling limits mycobacterial growth. Nature, 2015, 517(7536): 612-615. doi:10.1038/nature13967. |
| [8] | Sabir N, Hussain T, Mangi MH, et al. Matrix metalloproteinases: Expression, regulation and role in the immunopathology of tuberculosis. Cell Prolif, 2019, 52(4): e12649. doi:10.1111/cpr.12649. |
| [9] | Cleverley TL, Peddineni S, Guarner J, et al. The host-directed therapeutic imatinib mesylate accelerates immune responses to Mycobacterium marinum infection and limits pathology associated with granulomas. PLoS Pathog, 2023, 19(5): e1011387. doi:10.1371/journal.ppat.1011387. |
| [10] | 关艳敏, 白大鹏. 结核病宿主导向治疗药物机制的研究进展. 继续医学教育, 2022, 36(10):157-160. doi:10.3969/j.issn.1004-6763.2022.10.040. |
| [11] | Singh DK, Bhaskar A, Pahuja I, et al. Cotreatment With Clofazimine and Rapamycin Eliminates Drug-Resistant Tuberculosis by Inducing Polyfunctional Central Memory T-Cell Responses. J Infect Dis, 2023, 228(9): 1166-1178. doi:10.1093/infdis/jiad214. |
| [12] | Cerni S, Shafer D, To K, et al. Investigating the Role of Everolimus in mTOR Inhibition and Autophagy Promotion as a Potential Host-Directed Therapeutic Target in Mycobacterium tuberculosis Infection. J Clin Med, 2019, 8(2):232. doi:10.3390/jcm8020232. |
| [13] | Walsh KF, Mcaulay K, Lee MH, et al. Early Bactericidal Activity Trial of Nitazoxanide for Pulmonary Tuberculosis. Antimicrob Agents Chemother, 2020, 64(5):e01956-19. doi:10.1128/AAC.01956-19. |
| [14] |
Schiebler M, Brown K, Hegyi K, et al. Functional drug screening reveals anticonvulsants as enhancers of mTOR-independent autophagic killing of Mycobacterium tuberculosis through inositol depletion. EMBO Mol Med, 2015, 7(2): 127-139. doi:10.15252/emmm.201404137.
pmid: 25535254 |
| [15] | Stanley SA, Barczak AK, Silvis MR, et al. Identification of host-targeted small molecules that restrict intracellular Mycobacterium tuberculosis growth. PLoS Pathog, 2014, 10(2): e1003946. doi:10.1371/journal.ppat.1003946. |
| [16] | Boland R, Heemskerk MT, Forn-Cuni G, et al. Repurposing Tamoxifen as Potential Host-Directed Therapeutic for Tuberculosis. mBio, 2023, 14(1): e0302422. doi:10.1128/mbio.03024-22. |
| [17] | Ouyang Q, Zhang K, Lin D, et al. Bazedoxifene Suppresses Intracellular Mycobacterium tuberculosis Growth by Enhancing Autophagy. mSphere, 2020, 5(2):e00124-20. doi:10.1128/mSphere.00124-20. |
| [18] | Chung C, Silwal P, Kim I, et al. Vitamin D-Cathelicidin Axis: at the Crossroads between Protective Immunity and Pathological Inflammation during Infection. Immune Netw, 2020, 20(2): e12. doi:10.4110/in.2020.20.e12. |
| [19] | Juarez E, Carranza C, Sanchez G, et al. Loperamide Restricts Intracellular Growth of Mycobacterium tuberculosis in Lung Macrophages. Am J Respir Cell Mol Biol, 2016, 55(6): 837-847. doi:10.1165/rcmb.2015-0383OC. |
| [20] |
Abate G, Ruminiski PG, Kumar M, et al. New Verapamil Analogs Inhibit Intracellular Mycobacteria without Affecting the Functions of Mycobacterium-Specific T Cells. Antimicrob Agents Chemother, 2015, 60(3): 1216-1225. doi:10.1128/AAC.01567-15.
pmid: 26643325 |
| [21] | Hu S, He W, Du X, et al. Vitamin B1 Helps to Limit Mycobacterium tuberculosis Growth via Regulating Innate Immunity in a Peroxisome Proliferator-Activated Receptor-gamma-Dependent Manner. Front Immunol, 2018, 9: 1778. doi:10.3389/fimmu.2018.01778. |
| [22] | Zhang X, Ding G, Yang X, et al. Myriocin enhances the clea-rance of M.tuberculosis by macrophages through the activation of PLIN2. mSphere, 2024, 9(7):e0025724. doi:10.1128/msphere.00257-24. |
| [23] | Bohme J, Martinez N, Li S, et al. Metformin enhances anti-mycobacterial responses by educating CD8+ T-cell immunometabolic circuits. Nat Commun, 2020, 11(1): 5225. doi:10.1038/s41467-020-19095-z. |
| [24] | Singhal A, Jie L, Kumar P, et al. Metformin as adjunct antituberculosis therapy. Sci Transl Med, 2014, 6(263): 263ra159. doi:10.1126/scitranslmed.3009885. |
| [25] | Pahuja I, Verma A, Ghoshal A, et al. Biapenem, a Carbapenem Antibiotic, Elicits Mycobacteria Specific Immune Responses and Reduces the Recurrence of Tuberculosis. Microbiol Spectr, 2023, 11(4): e0085823. doi:10.1128/spectrum.00858-23. |
| [26] | Mayer-Barber KD, Andrade BB, Oland SD, et al. Host-directed therapy of tuberculosis based on interleukin-1 and type Ⅰ interferon crosstalk. Nature, 2014, 511(7507): 99-103. doi:10.1038/nature13489. |
| [27] |
Vilaplana C, Marzo E, Tapia G, et al. Ibuprofen therapy resulted in significantly decreased tissue bacillary loads and increased survival in a new murine experimental model of active tuberculosis. J Infect Dis, 2013, 208(2): 199-202. doi:10.1093/infdis/jit152.
pmid: 23564636 |
| [28] | Mishra R, Krishan S, Siddiqui AN, et al. Potential role of adjuvant drugs on efficacy of first line oral antitubercular therapy: Drug repurposing. Tuberculosis (Edinb), 2020, 120: 101902. doi:10.1016/j.tube.2020.101902. |
| [29] | Sorgi CA, Soares EM, Rosada RS, et al. Eicosanoid pathway on host resistance and inflammation during Mycobacterium tuberculosis infection is comprised by LTB(4) reduction but not PGE2 increment. Biochim Biophys Acta Mol Basis Dis, 2020, 1866(3): 165574. doi:10.1016/j.bbadis.2019.165574. |
| [30] |
Maitra A, Evangelopoulos D, Chrzastek A, et al. Carprofen elicits pleiotropic mechanisms of bactericidal action with the potential to reverse antimicrobial drug resistance in tuberculosis. J Antimicrob Chemother, 2020, 75(11): 3194-3201. doi:10.1093/jac/dkaa307.
pmid: 32790867 |
| [31] | Maiga M, Ammerman NC, Maiga MC, et al. Adjuvant host-directed therapy with types 3 and 5 but not type 4 phospho-diesterase inhibitors shortens the duration of tuberculosis treatment. J Infect Dis, 2013, 208(3): 512-519. doi:10.1093/infdis/jit187. |
| [32] |
Maiga MC, Ahidjo BA, Maiga M, et al. Roflumilast, a Type 4 Phosphodiesterase Inhibitor, Shows Promising Adjunctive, Host-Directed Therapeutic Activity in a Mouse Model of Tuberculosis. Antimicrob Agents Chemother, 2015, 59(12): 7888-7890. doi:10.1128/AAC.02145-15.
pmid: 26438491 |
| [33] |
Parihar SP, Guler R, Khutlang R, et al. Statin therapy reduces the mycobacterium tuberculosis burden in human macrophages and in mice by enhancing autophagy and phagosome maturation. J Infect Dis, 2014, 209(5): 754-763. doi:10.1093/infdis/jit550.
pmid: 24133190 |
| [34] |
Parihar SP, Guler R, Brombacher F. Statins: a viable candidate for host-directed therapy against infectious diseases. Nat Rev Immunol, 2019, 19(2): 104-117. doi:10.1038/s41577-018-0094-3.
pmid: 30487528 |
| [35] | Safe IP, Amaral EP, Araujo-Pereira M, et al. Adjunct N-Acetylcysteine Treatment in Hospitalized Patients With HIV-Associated Tuberculosis Dampens the Oxidative Stress in Peripheral Blood: Results From the RIPENACTB Study Trial. Front Immunol, 2020, 11: 602589. doi:10.3389/fimmu.2020.602589. |
| [36] | Shankaran D, Singh A, Dawa S, et al. The antidepressant sertraline provides a novel host directed therapy module for augmenting TB therapy. Elife, 2023, 12:e64834. doi:10.7554/eLife.64834. |
| [37] | Skerry C, Harper J, Klunk M, et al. Adjunctive TNF inhibition with standard treatment enhances bacterial clearance in a murine model of necrotic TB granulomas. PLoS One, 2012, 7(6): e39680. doi:10.1371/journal.pone.0039680. |
| [38] |
Maiga M, Ahidjo BA, Maiga MC, et al. Efficacy of Adjunctive Tofacitinib Therapy in Mouse Models of Tuberculosis. EBioMedicine, 2015, 2(8): 868-873. doi:10.1016/j.ebiom.2015.07.014.
pmid: 26425693 |
| [39] |
Young C, Walzl G, Du Plessis N. Therapeutic host-directed strategies to improve outcome in tuberculosis. Mucosal Immunol, 2020, 13(2): 190-204. doi:10.1038/s41385-019-0226-5.
pmid: 31772320 |
| [40] | Chandra P, Grigsby SJ, Philips JA. Immune evasion and provo-cation by Mycobacterium tuberculosis. Nat Rev Microbiol, 2022, 20(12): 750-766. doi:10.1038/s41579-022-00763-4. |
| [41] |
Orme IM, Robinson RT, Cooper AM. The balance between protective and pathogenic immune responses in the TB-infected lung. Nat Immunol, 2015, 16(1): 57-63. doi:10.1038/ni.3048.
pmid: 25521685 |
| [42] |
Ernst JD. Mechanisms of M.tuberculosis Immune Evasion as Challenges to TB Vaccine Design. Cell Host Microbe, 2018, 24(1): 34-42. doi:10.1016/j.chom.2018.06.004.
pmid: 30001523 |
| [43] |
Oehlers SH, Cronan MR, Beerman RW, et al. Infection-Induced Vascular Permeability Aids Mycobacterial Growth. J Infect Dis, 2017, 215(5): 813-817. doi:10.1093/infdis/jiw355.
pmid: 27496976 |
| [44] | Miow QH, Vallejo AF, Wang Y, et al. Doxycycline host-directed therapy in human pulmonary tuberculosis. J Clin Invest, 2021, 131(15):e141895. doi:10.1172/JCI141895. |
| [45] |
Flynn JL, Chan J. Immune cell interactions in tuberculosis. Cell, 2022, 185(25): 4682-4702. doi:10.1016/j.cell.2022.10.025.
pmid: 36493751 |
| [46] | Bo H, Moure UAE, Yang Y, et al. Mycobacterium tuberculosis-macrophage interaction: Molecular updates. Front Cell Infect Microbiol, 2023, 13: 1062963. doi:10.3389/fcimb.2023.1062963. |
| [47] |
Ersahin T, Tuncbag N, Cetin-Atalay R. The PI3K/AKT/mTOR interactive pathway. Mol Biosyst, 2015, 11(7): 1946-1954. doi:10.1039/c5mb00101c.
pmid: 25924008 |
| [48] |
Kinsey CG, Camolotto SA, Boespflug AM, et al. Protective autophagy elicited by RAF—>MEK—>ERK inhibition suggests a treatment strategy for RAS-driven cancers. Nat Med, 2019, 25(4): 620-627. doi:10.1038/s41591-019-0367-9.
pmid: 30833748 |
| [49] |
Sui X, Kong N, Ye L, et al. p38 and JNK MAPK pathways control the balance of apoptosis and autophagy in response to chemotherapeutic agents. Cancer Lett, 2014, 344(2): 174-179. doi:10.1016/j.canlet.2013.11.019.
pmid: 24333738 |
| [50] | Yang L, Wu Y, Lin S, et al. sPLA2-IB and PLA2R mediate insufficient autophagy and contribute to podocyte injury in idiopathic membranous nephropathy by activation of the p38MAPK/mTOR/ULK1(ser757) signaling pathway. FASEB J, 2021, 35(2): e21170. doi:10.1096/fj.202001143R. |
| [51] | Kim SY, Yang CS, Lee HM, et al. ESRRA (estrogen-related receptor alpha) is a key coordinator of transcriptional and post-translational activation of autophagy to promote innate host defense. Autophagy, 2018, 14(1): 152-168. doi:10.1080/15548627.2017.1339001. |
| [52] | 文章新, 刘红, 盛志峰, 等. 维生素D及其受体对糖尿病肾病保护作用的研究进展. 中国医师杂志, 2021, 23(12):1901-1904. doi:10.3760/cma.j.cn431274-20200907-01247. |
| [53] | Fabri M, Stenger S, Shin DM, et al. Vitamin D is required for IFN-gamma-mediated antimicrobial activity of human macrophages. Sci Transl Med, 2011, 3(104): 104ra102. doi:10.1126/scitranslmed.3003045. |
| [54] | Adams KN, Verma AK, Gopalaswamy R, et al. Diverse Clinical Isolates of Mycobacterium tuberculosis Develop Macrophage-Induced Rifampin Tolerance. J Infect Dis, 2019, 219(10): 1554-1558. doi:10.1093/infdis/jiy710. |
| [55] |
Adams KN, Szumowski JD, Ramakrishnan L. Verapamil, and its metabolite norverapamil, inhibit macrophage-induced, bacterial efflux pump-mediated tolerance to multiple anti-tubercular drugs. J Infect Dis, 2014, 210(3): 456-466. doi:10.1093/infdis/jiu095.
pmid: 24532601 |
| [56] | Lake MA, Adams KN, Nie F, et al. The human proton pump inhibitors inhibit Mycobacterium tuberculosis rifampicin efflux and macrophage-induced rifampicin tolerance. Proc Natl Acad Sci U S A, 2023, 120(7): e2215512120. doi:10.1073/pnas.2215512120. |
| [57] | Guirado E, Rajaram MV, Chawla A, et al. Deletion of PPARgamma in lung macrophages provides an immunoprotective response against M.tuberculosis infection in mice. Tuberculosis (Edinb), 2018, 111: 170-177. doi:10.1016/j.tube.2018.06.012. |
| [58] |
Sutter A, Landis D, Nugent K. Metformin has immunomodulatory effects which support its potential use as adjunctive therapy in tuberculosis. Indian J Tuberc, 2024, 71(1): 89-95. doi:10.1016/j.ijtb.2023.05.011.
pmid: 38296396 |
| [59] | Singh DK, Dwivedi VP, Ranganathan A, et al. Blockade of the Kv1.3 K+ Channel Enhances BCG Vaccine Efficacy by Expanding Central Memory T Lymphocytes. J Infect Dis, 2016, 214(9): 1456-1464. doi:10.1093/infdis/jiw395. |
| [60] | Pires D, Valente S, Calado M, et al. Repurposing Saquinavir for Host-Directed Therapy to Control Mycobacterium Tuberculosis Infection. Front Immunol, 2021, 12: 647728. doi:10.3389/fimmu.2021.647728. |
| [61] |
Cicchese JM, Evans S, Hult C, et al. Dynamic balance of pro- and anti-inflammatory signals controls disease and limits pathology. Immunol Rev, 2018, 285(1): 147-167. doi:10.1111/imr.12671.
pmid: 30129209 |
| [62] |
Zumla A, Rao M, Dodoo E, et al. Potential of immunomodulatory agents as adjunct host-directed therapies for multidrug-resistant tuberculosis. BMC Med, 2016, 14: 89. doi:10.1186/s12916-016-0635-1.
pmid: 27301245 |
| [63] | Gupta A, Misra A, Deretic V. Targeted pulmonary delivery of inducers of host macrophage autophagy as a potential host-directed chemotherapy of tuberculosis. Adv Drug Deliv Rev, 2016, 102: 10-20. doi:10.1016/j.addr.2016.01.016. |
| [64] | Van Toorn R, Zaharie SD, Seddon JA, et al. The use of thalidomide to treat children with tuberculosis meningitis: A review. Tuberculosis (Edinb), 2021, 130: 102125. doi:10.1016/j.tube.2021.102125. |
| [65] | 申晓娜, 姚岚. 结核病宿主导向治疗研究进展. 同济大学学报(医学版), 2019, 40(1):123-127. doi:10.16118/j.1008-0392.2019.01.023. |
| [1] | 中国防痨协会结核病控制专业分会, 中国防痨协会青年分会, 《中国防痨杂志》编辑委员会. 中国结核病数字服药依从性技术应用指南[J]. 中国防痨杂志, 2025, 47(4): 385-397. |
| [2] | 李锦浩, 胡冬梅, 徐彩红. 结核病防治医务工作者开展预防性抗结核治疗工作意愿调查及影响因素分析[J]. 中国防痨杂志, 2025, 47(4): 398-407. |
| [3] | 李玉红, 梅金周, 苏伟, 阮云洲, 刘玉舒, 赵雁林, 刘小秋. 2015—2021年全国65岁及以上老年利福平耐药肺结核患者治疗转归及影响因素分析[J]. 中国防痨杂志, 2025, 47(4): 408-415. |
| [4] | 姜雪, 白云龙, 马建军, 安源, 杨帆, 赵庆龙. 2020—2023年吉林省利福平耐药肺结核患者诊治延迟现状及影响因素分析[J]. 中国防痨杂志, 2025, 47(4): 416-424. |
| [5] | 吴璇, 张艳秋, 徐吉英, 孟丹, 孙定勇. 2019—2023年河南省肺结核合并糖尿病患者治疗转归影响因素分析[J]. 中国防痨杂志, 2025, 47(4): 425-431. |
| [6] | 安源, 白云龙, 赵庆龙, 马建军, 姜雪, 潘艳, 高迎, 高智慧. 2018—2022年吉林省肺结核合并糖尿病患者治疗转归情况及影响因素分析[J]. 中国防痨杂志, 2025, 47(4): 432-438. |
| [7] | 冯畏, 郑海伦, 孟炜丽, 罗萍. 2018—2023年北京市西城区结核病防治机构登记管理肺结核患者到位前漏报情况分析[J]. 中国防痨杂志, 2025, 47(4): 439-443. |
| [8] | 胡一凡, 杜博平, 吴亚东, 朱传智, 张蓝月, 贾红彦, 孙琦, 潘丽萍, 张宗德, 李自慧. Mce4C蛋白参与结核分枝杆菌摄取利用胆固醇的实验研究[J]. 中国防痨杂志, 2025, 47(4): 444-453. |
| [9] | 盛杰, 洪凯峰, 米尔扎提·艾沙, 唐伟, 地里下提·阿不力孜. 白细胞介素22和p38 MAPK信号通路抑制骨关节结核骨质破坏的作用机制研究[J]. 中国防痨杂志, 2025, 47(4): 454-459. |
| [10] | 王颖超, 刘唯夷, 姬秀秀, 尚雪恬, 贾红彦, 张蓝月, 孙琦, 杜博平, 朱传智, 潘丽萍, 张宗德. 结核病患者外周血单个核细胞内环状RNA表达谱分析及诊断标识的鉴定[J]. 中国防痨杂志, 2025, 47(4): 460-470. |
| [11] | 朱明智, 邵燕琴, 范大鹏, 刘立宾, 梅宾, 戴玲珊, 蔡龙. 尿液脂阿拉伯甘露聚糖抗原检测对肺外结核的诊断价值[J]. 中国防痨杂志, 2025, 47(4): 471-476. |
| [12] | 郝明晓, 米洁, 许宗仪. 延续性护理路径在结核性脑膜炎患者中的应用效果分析[J]. 中国防痨杂志, 2025, 47(4): 477-481. |
| [13] | 尚希钰, 张慧芳, 曹玉清, 熊一白, 纪鑫毓, 田雅欣, 李佳佳, 王倪, 马艳. 基于文献计量学的结核病中医药基础研究全球研究现状及热点分析[J]. 中国防痨杂志, 2025, 47(4): 482-497. |
| [14] | 秦丽莉, 杨澄清, 麦洪珍, 徐齐峰, 薛新颖, 路希维. 结核后肺曲霉病的临床诊疗研究进展[J]. 中国防痨杂志, 2025, 47(4): 498-504. |
| [15] | 罗莉, 罗林紫, 尹曲华, 周磊, 卢志斌, 丁衍, 肖阳宝. 淋巴结瘘型气管支气管结核的支气管镜下诊疗进展[J]. 中国防痨杂志, 2025, 47(4): 505-512. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
 京公网安备11010202007215号
ip访问总数: ip当日访问总数: 当前在线人数:
京公网安备11010202007215号
ip访问总数: ip当日访问总数: 当前在线人数:
 本作品遵循Creative Commons Attribution 3.0 License授权许可
本作品遵循Creative Commons Attribution 3.0 License授权许可